WELCOME FROM CHAIRMAN –
Eric EvansFor over 50 years the Orthopaedic Institute has funded research and education to improve the treatment of patients with conditions that affect the musculo-skeletal system at the Robert Jones & Agnes Hunt Orthopaedic Hospital Foundation Trust, a long-standing centre of excellence in world orthopaedics.
It is pleasing to report that although research studies and teaching were severely affected by the pandemic, both areas are now fully restored to full capacity and continue to develop with many innovative research projects and more training courses being held, funded through us by external Charitable Trusts, Foundations, patients and members of the public. We are extremely grateful for the support received year on year which enables us to continue with these vital services.
It is also pleasing to see that many research initiatives instigated with the support of the Orthopaedic Institute are thriving and now in their post-research phase, have been integrated into the core clinical work of the hospital.
Administration
There were no changes in the Board of Directors during the current year.
The financial standing of the Institute remains sound and we are indebted to our treasurer Louise Osselton and bookkeeper Fiona Bain for their careful management of our resources. The Board keeps a watch on the management of our investments and is satisfied with the current performance.
Judy Harris continues to provide administrative support to the board and we are grateful for the care and attention that she brings to the post.
We welcomed our new Course Organiser, Laura Haythorn during the year. Laura has worked hard in effectively reinstating and bringing in a number of new courses working with our clinical colleagues, after the inevitable disruption and restrictions caused by the pandemic. Ongoing continued development of our flagship courses is progressing to reflect the changes in Postgraduate medical education in the NHS. Laura will work with our trainers to ensure that Oswestry maintains its renowned reputation.
Debra Alexander has had a successful, albeit challenging year in her role as Fundraiser. Again, the pandemic severely restricting fund-raising activities. The Annual Snowpaedic Challenge, a sponsored hike up Snowdon for patients, staff and supporters, was held in September although with fewer participants than we have previously enjoyed. Donations to support research projects and items of laboratory equipment have continued and we are grateful to the external Trusts, Foundations and Charities that have supported our requests.
Research
Many thanks go to Dr Robin Butler for standing in as Acting Chairman of the Panel who stood down for personal reasons during the year. We welcome Teresa Jones as the new Chair. Teresa comes with wealth of knowledge gained during her previous career in Research Management. The Panel continues to perform its duty of providing peer review for projects submitted for funding and monitoring their progress.
Throughout the year 2022-2023 the Institute has supported a number of research projects, with many more in the pipeline. The range of research is impressive, varying from clinical trials in common orthopaedic problems to molecular biology approaches and to less common forms of muscular dystrophy. Also, from radiological studies on patients with back pain to gait analysis in children with cerebral palsy. The unifying factors are that they are all well designed studies on conditions affecting patients attending our hospital.
We have also provided funding to purchase and maintain new pieces of laboratory equipment and awarded 24 grants to cover a variety of specialist training courses, publishing fees and placements for upcoming PhD student ‘scientists’ of tomorrow.
Research Day held on Friday 27th April in tandem with the Specialist Orthopaedic Registrars was a stimulating day and our thanks go to all who contributed.
Teaching
The Institute has started again to convene courses in the review period after our enforced furlough and we are grateful to the convenors and faculty of each for the work they put in.
Our flagship courses, the Clinical Examination and Viva Courses, have earned world-class reputations and delegates consider them to be the ‘best of their kind’ and as new delegates were eager to book, we were pleased to run the Clinical Examination course again in October.
The reputation of the courses has been built on the participation of a huge variety of model patients and the commitment of the highest quality Lecturers and Examiners and we are grateful to all involved.
Current Projects
The Institute has excellent relations with the leadership team of the RJAH Foundation Trust and is working with them, within its charitable aims, to take forward important initiatives for the future.
Veteran’s Outpatient Centre
The Headley Court Veteran’s Orthopaedic Centre for which the Orthopaedic Institute provided the initial impetus and funding, was opened by Sophie, the Duchess of Edinburgh in May 2023 having been supported by the Headley Court Charity. We are very proud to hold the Bronze Award for the support we provide to our Veteran’s.
Cell therapy unit
Fully financed by the Orthopaedic Institute over twenty years ago, the Oscell Cell Therapy Unit provides cells for clinical trials to repair damaged joint cartilage. Changes to the regulatory framework under which cells are produced have required modification and extension of the facility. The Institute has supported this and a numbers of studies and will continue to assist in the long-term development of cell therapies.
Education/Training Centre
The Institute has worked with the hospital to upgrade our current Lecture theatre and Library, but it is clear that a new centre will be needed in the near future to allow an expansion of training for all clinical specialties. The Institute funded an options review, being the first stage of a business plan for the project. We look forward to supporting this venture as ideas to maximise the number of courses and training available to colleagues and allied professionals from across the globe progresses.
In conclusion
This report provides a flavour of the innovation and precision of the research being carried out by the clinicians and scientists at the Robert Jones & Agnes Hunt Orthopaedic Hospital NHS Foundation Trust.
The Orthopaedic Institute provides the financial support sought by researchers to get projects started and through to proof of concept phase. We also play an important role in providing the technology to keep our researchers at the cutting edge.
Please help us help them – together we have a great record of success.
Chairman’s Report
For over 50 years the Orthopaedic Institute has funded research and education to improve the treatment of patients with conditions that affect the musculo-skeletal system at the Robert Jones & Agnes Hunt Orthopaedic Hospital Foundation Trust, a long-standing centre of excellence in world orthopaedics.
It is pleasing to report that although research studies and teaching were severely affected by the pandemic, both areas are now fully restored to full capacity and continue to develop with many innovative research projects and more training courses being held, funded through us by external Charitable Trusts, Foundations, patients and members of the public. We are extremely grateful for the support received year on year which enables us to continue with these vital services.
It is also pleasing to see that many research initiatives instigated with the support of the Orthopaedic Institute are thriving and now in their post-research phase, have been integrated into the core clinical work of the hospital.
Administration
There were no changes in the Board of Directors during the current year.
The financial standing of the Institute remains sound and we are indebted to our treasurer Louise Osselton and bookkeeper Fiona Bain for their careful management of our resources. The Board keeps a watch on the management of our investments and is satisfied with the current performance.
Judy Harris continues to provide administrative support to the board and we are grateful for the care and attention that she brings to the post.
We welcomed our new Course Organiser, Laura Haythorn during the year. Laura has worked hard in effectively reinstating and bringing in a number of new courses working with our clinical colleagues, after the inevitable disruption and restrictions caused by the pandemic. Ongoing continued development of our flagship courses is progressing to reflect the changes in Postgraduate medical education in the NHS. Laura will work with our trainers to ensure that Oswestry maintains its renowned reputation.
Debra Alexander has had a successful, albeit challenging year in her role as Fundraiser. Again, the pandemic severely restricting fund-raising activities. The Annual Snowpaedic Challenge, a sponsored hike up Snowdon for ex-patients, staff and supporters, was held in September although with fewer participants than we have previously enjoyed. Donations to support research projects and items of laboratory equipment have continued and we are grateful to the external Trusts, Foundations and Charities that have supported our requests.
Research
Many thanks go to Dr Robin Butler for standing in as Acting Chairman of the Panel who stood down for personal reasons during the year. We welcome Teresa Jones as the new Chair. Teresa comes with wealth of knowledge gained during her previous career in Research Management. The Panel continues to perform its duty of providing peer review for projects submitted for funding and monitoring their progress.
Throughout the year 2022-2023 the Institute has supported a number of research projects, with many more in the pipeline. The range of research is impressive, varying from clinical trials in common orthopaedic problems to molecular biology approaches and to less common forms of muscular dystrophy. Also, from radiological studies on patients with back pain to gait analysis in children with cerebral palsy. The unifying factors are that they are all well designed studies on conditions affecting patients attending our hospital.
We have also provided funding to purchase and maintain new pieces of laboratory equipment and awarded 24 grants to cover a variety of specialist training courses, publishing fees and placements for upcoming PhD student ‘scientists’ of tomorrow.
Research Day held on Friday 27th April in tandem with the Specialist Orthopaedic Registrars was a stimulating day and our thanks go to all who contributed.
Teaching
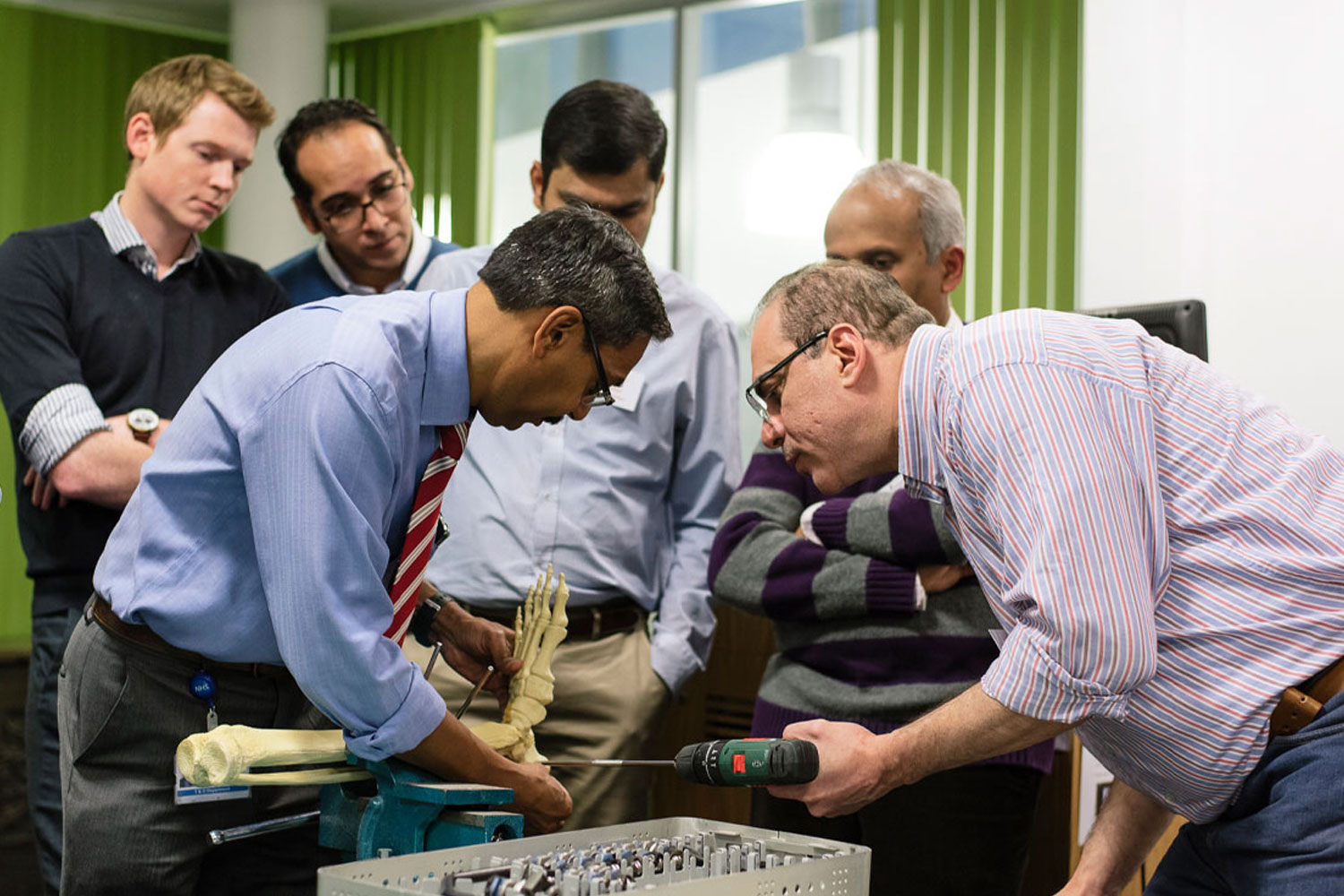
The Institute has started again to convene courses in the review period after our enforced furlough and we are grateful to the convenors and faculty of each for the work they put in.
Our flagship courses, the Clinical Examination and Viva Courses, have earned world-class reputations and delegates consider them to be the ‘best of their kind’ and as new delegates were eager to book, we were pleased to run the Clinical Examination course again in October.
The reputation of the courses has been built on the participation of a huge variety of model patients and the commitment of the highest quality Lecturers and Examiners and we are grateful to all involved.
Current Projects
The Institute has excellent relations with the leadership team of the RJAH Foundation Trust and is working with them, within its charitable aims, to take forward important initiatives for the future.
Veteran’s Outpatient Centre
The Headley Court Veteran’s Orthopaedic Centre for which the Orthopaedic Institute provided the initial impetus and funding, was opened by Sophie, the Duchess of Edinburgh in May 2023 having been supported by the Headley Court Charity. We are very proud to hold the Bronze Award for the support we provide to our Veteran’s.
Cell therapy unit
Fully financed by the Orthopaedic Institute over twenty years ago, the Oscell Cell Therapy Unit provides cells for clinical trials to repair damaged joint cartilage. Changes to the regulatory framework under which cells are produced have required modification and extension of the facility. The Institute has supported this and a numbers of studies and will continue to assist in the long-term development of cell therapies.
Education/Training Centre
The Institute has worked with the hospital to upgrade our current Lecture theatre and Library, but it is clear that a new centre will be needed in the near future to allow an expansion of training for all clinical specialties. The Institute funded an options review, being the first stage of a business plan for the project. We look forward to supporting this venture as ideas to maximise the number of courses and training available to colleagues and allied professionals from across the globe progresses.
In conclusion
This report provides a flavour of the innovation and precision of the research being carried out by the clinicians and scientists at the Robert Jones & Agnes Hunt Orthopaedic Hospital NHS Foundation Trust.
The Orthopaedic Institute provides the financial support sought by researchers to get projects started and through to proof of concept phase. We also play an important role in providing the technology to keep our researchers at the cutting edge.
Please help us help them – together we have a great record of success.
Eric Evans – Chairman
Administration
There were no changes in the Board of Directors during the current year.
The financial standing of the Institute remains sound and we are indebted to our treasurer Louise Osselton and bookkeeper Fiona Bain for their careful management of our resources. The Board keeps a watch on the management of our investments and is satisfied with the current performance.
Judy Harris continues to provide administrative support to the board and we are grateful for the care and attention that she brings to the post.
We welcomed our new Course Organiser, Laura Haythorn during the year. Laura has worked hard in effectively reinstating and bringing in a number of new courses working with our clinical colleagues, after the inevitable disruption and restrictions caused by the pandemic. Ongoing continued development of our flagship courses is progressing to reflect the changes in Postgraduate medical education in the NHS. Laura will work with our trainers to ensure that Oswestry maintains its renowned reputation.
Debra Alexander has had a successful, albeit challenging year in her role as Fundraiser. Again, the pandemic severely restricting fund-raising activities. The Annual Snowpaedic Challenge, a sponsored hike up Snowdon for patients, staff and supporters, was held in September although with fewer participants than we have previously enjoyed. Donations to support research projects and items of laboratory equipment have continued and we are grateful to the external Trusts, Foundations and Charities that have supported our requests.
Research
Many thanks go to Dr Robin Butler for standing in as Acting Chairman of the Panel who stood down for personal reasons during the year. We welcome Teresa Jones as the new Chair. Teresa comes with wealth of knowledge gained during her previous career in Research Management. The Panel continues to perform its duty of providing peer review for projects submitted for funding and monitoring their progress.
Throughout the year 2022-2023 the Institute has supported a number of research projects, with many more in the pipeline. The range of research is impressive, varying from clinical trials in common orthopaedic problems to molecular biology approaches and to less common forms of muscular dystrophy. Also, from radiological studies on patients with back pain to gait analysis in children with cerebral palsy. The unifying factors are that they are all well designed studies on conditions affecting patients attending our hospital.
We have also provided funding to purchase and maintain new pieces of laboratory equipment and awarded 24 grants to cover a variety of specialist training courses, publishing fees and placements for upcoming PhD student ‘scientists’ of tomorrow.
Research Day held on Friday 27th April in tandem with the Specialist Orthopaedic Registrars was a stimulating day and our thanks go to all who contributed.
Teaching
The Institute has started again to convene courses in the review period after our enforced furlough and we are grateful to the convenors and faculty of each for the work they put in.
Our flagship courses, the Clinical Examination and Viva Courses, have earned world-class reputations and delegates consider them to be the ‘best of their kind’ and as new delegates were eager to book, we were pleased to run the Clinical Examination course again in October.
The reputation of the courses has been built on the participation of a huge variety of model patients and the commitment of the highest quality Lecturers and Examiners and we are grateful to all involved.
Fundraising
With an ever decreasing amount of charitable funds available we are extremely grateful to all our sponsors including Grant Giving Charities, Corporate Companies and Individuals for their kind and generous contributions to the Orthopaedic Institute. This allows us to continue to support the vital Research and Training here at the Robert Jones & Agnes Hunt Orthopaedic Hospital.
In Conclusion
This report provides a flavour of the innovation and precision of the research being carried out by the clinicians and scientists at the Robert Jones & Agnes Hunt Orthopaedic Hospital NHS Foundation Trust.
The Orthopaedic Institute provides the financial support sought by researchers to get projects started and through to proof of concept phase. We also play an important role in providing the technology to keep our researchers at the cutting edge.
Please help us help them – together we have a great record of success.
Eric Evans – Chairman, Orthopaedic Institute Ltd
Who’s who

Eric Evans
Chairman
Read Bio
Now widowed with one son, I was originally educated at Wrekin College, Wellington, thence studying business management in Coventry. I worked for Rootes Motors for a number of years in varying positions around the UK. I returned to Oswestry, owning and running a retail motor franchise representing Peugeot until retiring in 2008.
I was interested in becoming a Trustee, when invited, as I hoped to bring a broader range of commercial experience to the running and administration of the Trust.
I was one of the initial members helping to establish Oswestry Rugby Club and still enjoy watching rugby and supporting Wales, especially in Cardiff. I have a lifelong interest in messing about in boats of all shapes and sizes, and thoroughly enjoyed cruising the Scottish Islands and South and West coasts of Ireland.

Louise Osselton
Treasurer
Read Bio
I qualified as a Chartered Accountant in 2007, having worked mainly in audit throughout my training and since qualifying. I have moved between jobs and across the country but settled back to the Oswestry area in 2014 to be close to family, having grown up near the Orthopaedic Hospital, and give our children stability for schooling. I am a director of CBSL Accountants, an independent accountancy practice based in Shrewsbury, where we have a broad mixture of clients from owner-managed family run local businesses to international groups – I love the challenge and variety of my role, working with a great team and building strong relationships with our clients and their families.
My work passion throughout my training and to date is working with charities – from audits and independent examinations to preparing accounts for charities and working with Trustees to look at controls and management reporting. I am fortunate to have worked at accountancy practices in both Cambridge and Oxford, where I worked with a considerable range of charities and university affiliates, many of which were involved with research and training.
I enjoy being involved with the Orthopaedic Institute – as a local charity that focuses on research and training with a leading reputation. Its also really interesting to be on the other side of the table being audited rather than auditor & understanding first-hand the challenges facing Trustees and our members.

Prof Wagih Shafik El Masri
Trustee
Read Bio
FCCS Ed, FRCP
Hon. Clinical Professor of Spinal Injuries (SI), Keele University
WSEM trained in Spinal Injuries and the allied surgical specialities in the Oxford Group of hospitals, Guys Hospital, Stoke Mandeville hospital and the USA between 1971 & 1983. He was appointed Consultant Surgeon in Spinal Injuries and Director of the Midland Centre for Spinal Injuries (MCSI) at the RJAH 1983. He personally treated and provided ongoing total care to about 10,000 patients with and without Spinal Cord damage. Between 1983 & 2000 he raised £6 million from Charity to rebuild and equip the MCSI in order to ensure a safe and fit for purpose environment for patients and staff and in collaboration with the scientists of the Institute to carry out research on regeneration of the injured spinal cord.
He published over 140 manuscripts, lectured worldwide, contributed to the National Health Service Framework and to the National Institute of Excellence (NICE). He is Past President of the International Spinal Cord Society and Past Chairman of the British Association of Spinal Cord Injury Specialists. He advised and prepared a report on Spinal Injuries for the WHO and won many National and International awards.
WEM and the service of the MCSI are acknowledged nationally and internationally for their excellence and contribution to knowledge, teaching, training and research in the field of Spinal Injuries and have been quoted the in House of Lords Parliamentary Debates as examples of good practice (Hansard) 8th April 2003, vol 647, no.79, p204; 9th March 2006 vol 679, no 117, p88 and 28th February 2009
The Midland Centre for Spinal Injuries (MCSI) is unique in being the only Centre in England with an active basic research science department in in the same hospital. The support of the Institute of Orthopaedics to both the MCSI and the research department has benefited both from a very successful collaboration that resulted in a number of publications that have added value and knowledge to both fields. WSEM believes that with support to the Institute further good collaborative work can improve both the management of the patient as well as our scientific knowledge
WSEM is married to Bettina who is a paediatric oncologist and they have one daughter Hannah May Emmeline who has graduated from Kings College Medical School in London and is hoping to serve as a General Practitioner.

Val Edwards
Trustee
Read Bio
Val is a local girl – born and bred in Trefonen near Oswestry where her family have lived for many generations. She still lives there as does one of her sons and she feels a very strong connection to the local community. She attended the local village school and then Bellan House Preparatory School. From age 11 she attended Oswestry Girls High School and after O levels and A levels she took a law degree at the University College of Wales Aberystwyth.
She completed her legal studies at College of Law Chester and then trained at Hatchers Solicitors. Over 40 years later she is still a partner there!! She specialises in commercial and agricultural property law and has wide experience of both. She is also involved in the management of Hatchers and runs the firm’s marketing and property needs. She is President of the Shrewsbury Business Chamber and a member of the local Bank of England Panel.
Val’s Grandfather was badly injured in WW1 and received much of his treatment at the Orthopaedic. They literally saved his life! The hospital and the research work it does have therefore always been close to her heart and it was for that reason she accepted the invitation to become a Trustee.
Val has three adult children and four small grandchildren. She is very much a country girl and is never happier than when she’s out in the fields. Horses have always played a major part in her life. Although she does not ride very often these days, she breeds sports ponies and loves spending time with her youngsters. All of Val’s children have competed since Pony Club days and one of her proudest moments was when they rode in the Prince Philip Cup at the Horse of the Year Show.
Val’s children continue to compete in Mounted Games (an obscure but hugely enjoyable equestrian sport) and she is an international judge, past Chairman of Great Britain and a representative of it on the British Equestrian Federation Council. Her her two sons have been top international riders and have won both the World and European Championships. . Val loves going to the cinema and tries to see all of the Oscar nominated films each year. Any time left is spent in her garden and kitchen.

Dr Brian Ashton
Trustee
Read Bio
Brian studied biochemistry at the University of Wales (Bangor) and undertook his doctoral work on skeletal proteins at the University of Oxford. His post-doctoral work at the University of Munster, Germany and the MRC Bone Research Lab in Oxford focussed on stem cells in bone marrow.
In 1985, Brian moved to the Robert Jones & Agnes Hunt Orthopaedic Hospital to become the Head of Arthritis Research. The Orthopaedic Institute helped enormously to develop the research laboratories at the hospital, and in 1996, following a national appeal run by the charity, the Leopold Muller Arthritis Research Centre was opened. The new facilities allowed them to recruit and train excellent researchers working on projects as diverse as the mechanisms of the movement of blood cells into joints of patients with inflammatory arthritis and the behaviour of stem cells and cartilage cells grown in culture. Working with orthopaedic surgeon Prof James Richardson, and with the support of the Orthopaedic Institute, he set up the cell therapy facility at the hospital, the only one of its kind in the UK, producing cells used clinically to repair damaged cartilage.
Brian became a director of the Orthopaedic Institute in 1996 and in 2014 became Chairman, taking over from Robert Parry who had to step down suddenly for family health reasons. Having seen the benefits that the charity has given in the promotion and development of research, teaching and learning, it has been a pleasure for him to take the responsibility of leading the charity until stepping down in September 2020.

Richard Lumby
Trustee
Read Bio
I am a Chartered Civil Engineer and spent my whole career working in Infrastructure Engineering, Construction and Facilities Management, from delivery of projects and services through to management of businesses in these sectors of industry.
I have lived in the Oswestry area since the mid 1980’s and always felt pride in the area’s association with the Robert Jones and Agnus Hunt Hospital and it’s position as a world class centre of Orthopaedics. When introduced to the Orthopaedic Institute by another Trustee I became interested in the importance of it’s work and the essential role that RJAH based research and education has on the continued success of the hospital and broader contribution to development in the Orthopaedic practice.
I settled in the Oswestry area in the mid 1980 having moved to work on the construction of the Oswestry Bypass and now live with my wife in West Felton. We had three daughters with one of them now working at the RJAH. I still work in the construction industry and also sit on the Shropshire Business Board. I am a keen Rugby enthusiast, sail, cycle and walk to keep fit and with my wife travel whenever we can.

Prof Sally Roberts
Trustee
Read Bio
PhD
Being a local yokel, I was born, bred and educated largely in and around Oswestry.
Starting work in RJAH in 1980 in Mr Norman Nisbet’s Charles Salt Centre, I began a long tradition of working with surgeons, firstly the spine surgeons, Mr John O’Brien (Jack the Back!)and then Professor Stephen Eisenstein before linking up with Professor James Richardson and his successors, Pete Gallacher and Paul Jermin.
I undertook my PhD on hip osteoarthritis at Birmingham University during this time and subsequently the hospital has linked up with Keele University.
Research interests are generally cartilage based, understanding its biology and function, what leads to its demise and how we can turn back the clock and repair or regenerate it when it goes wrong.
Having been very fortunate to have had the support of the Orthopaedic Institute Ltd for our group’s research over the years, it is an honour to have become a Trustee.

Robert Freeman
Trustee
Read Bio

Stephen Bratt
Trustee
Read Bio

Debra Alexander
Fundraiser
Read Bio
My career path through BT led me to work as a Business Sales Administration Manager for a number of years then moving into Event Management as an Operations Director before relocating back to Shropshire.
In my spare time I love to walk, ride, dance, cook and spend time with family and friends.

Laura Haythorn
Course Organiser
Read Bio
I am the Orthopaedic Institute’s Course Organiser, organising some 26 clinical courses each year. The majority of my career for 10 years was in the private education sector , where I worked with younger children & also ran the international holiday club. My most recent role was very different where I moved to the travel industry and was an assistant manager in a independant travel agents.
I have lived in and around Oswestry throughout my life, and have always felt very lucky to live in such a beautiful part of the country. When I am not working, myself and my family enjoy exploring new places, we also like travelling abroad.
I am married with a 2 Year Old Son Albert.
Judith Harris
Administrator
Read Bio
I am the Institute Administrator and work for the Orthopaedic Institute Ltd on an ad hoc basis. My main job is that of Postgraduate Administrator and my role is to assist the Core Members of the Training Committee to provide a quality service in postgraduate medical education and training within the Trust, thus, enabling orthopaedic trainees to gain the relevant competences, knowledge, skills, attitudes and experience to pass the Intercollegiate Exams, achieve their Certificate of Completion of Training (CCT) and become competent NHS Consultant Staff, delivering safe and effective patient care.
I have worked at the Trust since 1981 in various Departments; firstly in the Administration Department, secondly as PA to the Principal of the School of Physiotherapy. I have been in my current role, which has developed over the years, since 1983.
When not working I enjoy socialising with friends and family, cross country fence judging for British Eventing and travelling.
I am married with a grown-up son.